Managing drainage systems
Different systems are available for urine drainage for patients with long-term urinary catheters.
Task 2
1 |

Closed drainage system - (c)Sue Woodward

Link drainage system - (c)Sue Woodward
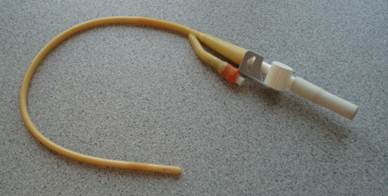
Catheter valve - (c)Sue Woodward
Whichever system is used, the device that is attached to the catheter should remain in situ and the connection should not be broken for five to seven days, or according to the manufacturers' instructions. Maintaining a sterile, continuously closed drainage system has been shown in a number of studies to reduce the risk of CAUTI (NICE, 2012) and NICE recommends staff should "Leave the closed system alone!" (NICE, 2012: p138).
Consider for a moment if you have ever seen a patient mobilising with a zimmer frame and a 2 litre urine drainage bag hanging from a stand on the front of the frame. Sadly this is not an uncommon sight in a variety of care settings and yet this is wholly inappropriate - urine will not flow uphill, so the drainage is ineffective and it does nothing to protect the patient's dignity!
Task 3
2 |
Reflux of urine is associated with infection, so drainage bags should be positioned in a way that prevents back-flow urine (NICE, 2012). Two litre drainage bags contain a "flutter valve" where the tubing is inserted into the bag. This consists in essence of two pieces of plastic (blue colour in figure 4) that are held together by surface tension. If the level of urine reaches the level of the flutter valve, it can float open and reflux can occur.

Flutter valve - (c) Sue Woodward
Task 4
3 |
The bag must never be put onto the bed or trolley with the patient, for example if a patient is being transferred or transported to another department - this increases the potential for reflux and backflow of old urine into the tubing.
Emptying the drainage bag also requires consideration, although again recommendations are made on the basis of expert consensus rather than research evidence (NICE, 2012).
Task 5
4 |
Staff emptying a drainage bag must ensure that correct hand decontamination technique is followed before and after manipulating any urine drainage bag (NICE, 2012). Non-sterile gloves and a clean plastic apron should be worn to protect the nurse or carer from contamination with body fluids as well as to protect the patient from cross-infection. A clean jug should be used for each patient.