Scenario Development

James Black
58, Male
Further details below...
Explanation
If a patient is symptomatic and the heart rate is controlled (<110 bpm) on medication, often a trial of a period in normal rhythm might make a patient feel better. Shocking the heart into sinus rhythm is tried first. This is termed electrical cardioversion. A synchronised DC shock (current delivered at the same time as the R wave of a QRS complex) is delivered to the heart which stuns the heart electrically and resets the automaticity of the heart so that the sinus node can take over again. It is important to synchronise the delivered current with the R wave to prevent shocks occurring during repolarisation which can initiate fibrillation of the ventricle leading to a cardiac arrest! It is also important to ensure the patient has had a period of anticoagulation to ensure no blood clot has formed in the atria. There is a theoretical risk of dislodging a clot once the patient’s atria start to contract normally. If the patient feels well after cardioversion to sinus rhythm they should stay on longterm anticoagulation as they can revert to AF sometimes without being aware.
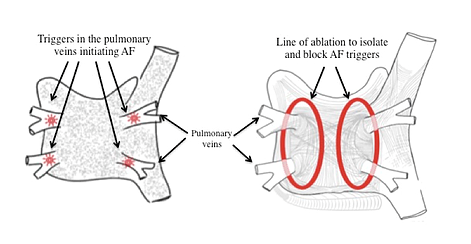
Ablation of the abnormal areas in the atria where the fibrillation waves are generated can also be performed. Often the areas around the entrance to the pulmonary veins that empty into the left atrium are susceptible to generating the abnormal rhythms and by creating scar tissue around these veins you can isolate the electrical conduction from these areas to allow the sinoatrial node to kick in and regulate atrial depolarisation.
Source: https://www.cardiacarrhythmiaassoc.com/cryoablation