Strategies for addressing barriers
Do you feel despondent?
-
Do patients listen?
A study in the New England Journal of Medicine showed that approximately one in five patients achieves and maintains a clinically significant amount of weight loss after a single behavioural intervention. This number doubles if follow up is provided, either through remote or person-to-person means. -
Why lose weight?
What are the health benefits of losing a modest amount of weight? These include reduced risk of high blood pressure, heart disease, stroke, type 2 diabetes, some types of cancer, infertility, osteoarthritis, back pain and depression. For example a man with BMI 40 who has modest 5% reduction in weight can expect at 12% reduction in his mortality risk. -
Is this my role?
Role modelling has been identified as an important part of the development of professional identity. If senior healthcare professionals don’t engage in treating the causes of ill health as well as treating the consequences, their trainees may question their role. If you are a trainee and this is important to you, can you find peers who also want to introduce this into their practice, and reflect on your developing role with them? - Can I do it?
Module two will help you to develop your motivational interviewing and behavioural change consultation techniques, giving you the resources and skills to support your patients.
Is fear of offense a problem?
-
Be sensitive to your patient's agenda
Your patient will have come to see you with their own agenda and expectations of the consultation. Addressing their weight may be part of your management of the patient's problem, in which case it is generally appropriate to raise the issue. To be proactive though it is important to be able to raise the issue in unrelated circumstances, however, there are still circumstances where it may be in inappropriate to raise the issue, for example consultations where emotions are running high, which you should be sensitive to. -
Put the patient in control
If you begin by simply offering the patient the chance to talk about their weight, using phrases such as "would you like to talk about your health in general?" "can I ask you about your weight?" "Do you have any concerns about your weight?" this leaves the patient in control. If the patient doesn't want to continue, then understand their position and roll with resistance, leaving the door open for a conversation on another day. -
Be non-judgemental but direct
Patients generally welcome the opportunity to talk about their weight, but dislike being judged by their appearance. A direct, supportive, inquisitive approach such as "how is your weight going at the moment?" works better than an indirect but advice heavy approach such as "according to my notes you are overweight, I advise you to lose weight". -
Your fear or theirs?
The fear of broaching a socially taboo topic is universal, and it is one of the reasons why some clinicians find it difficult to strike up conversations about planning for death with patients. However, research shows that patients often want to talk about these topics with their doctors but are struggling to raise the issue themselves. Simply letting patients know that you are ready and open to having that conversation with them is helpful.
Is time a problem?
Broach and book
Ask the patient if they would like to talk about their weight and if they are concerned about their weight – if they are, book a separate appointment to discuss in more depth with resources such as a food diary to take away with them. Here is a typical way of broaching and booking a further appointment.
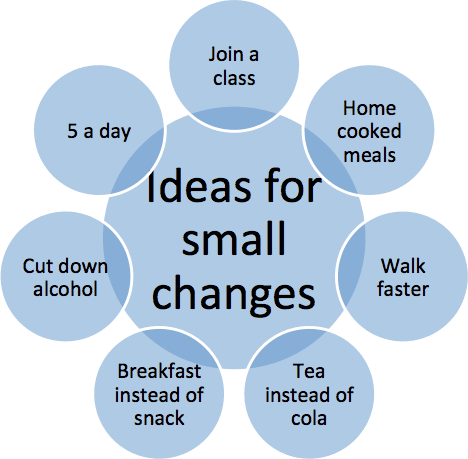
Small steps
Encourage patients to think of one single small step that they can take to improve their health. Use a phrase such as "can you think of one small thing to improve your diet or increase the amount of exercise that you take?". You can suggest options with phrases such as "some people find x helpful because of y, what do you think about that?", but avoid phrases such as "I suggest that you x". Help them to plan and problem solve. Make a note to ask how they did next time you see them.
Teamwork
Ask the patient if they would like to talk about their weight and are concerned about their weight – if they are, involve another member of your team to take the matter further. Recently trained or trainee nurses, doctors, pharmacists, OTs, and physios may all have had some degree of training on obesity in their undergraduate training, and many senior members of staff will have attended post graduate or vocational training.
Prepared resources
Have a selection of prepared information leaflets that you can offer to patients at hand. Again broach and ask about the patient's concerns, then give them a leaflet and ask them to keep a food diary; ask them to be honest with the diary so that you can work on genuine changes together, and review when you next see them.