Moving forward 
Read about how these healthcare professionals have begun to develop their practice and address the issues that they raised at the start of the module.
The hospital doctor

Peter is a speciality trainee working in acute medicine and cardiology. He estimates that obesity has contributed to the presentation of at least 10% of the patients in his acute medical unit, yet has never seen his consultant or team raise the issue with his patients [role modelling]. He explains:
“My colleagues and I get frustrated at obesity never being mentioned on our ward rounds, [addressing lack or role modelling] so we decided to get together and discuss how to tackle this. We have to assess every patient on admission for smoking and offer smoking cessation support so we are now combing this with having a conversation about weight [addressing time pressures]. We have found that our patients are often shaken by the fact that they have been admitted and are concerned about the effect that their lifestyle choices [addressing fear of offense and role legitimacy] have had on their health and are very open to talking about their problems. We now simply put "patient has requested support for weight loss" onto their discharge summary under the Actions for GP section [addressing time pressures].”
The general practitioner

Dr Barker has seen as dramatic increase in the number of obese patients on her practice list since she completed her training and is concerned about the future impact on health services, but is unsure of how best this should be addressed.
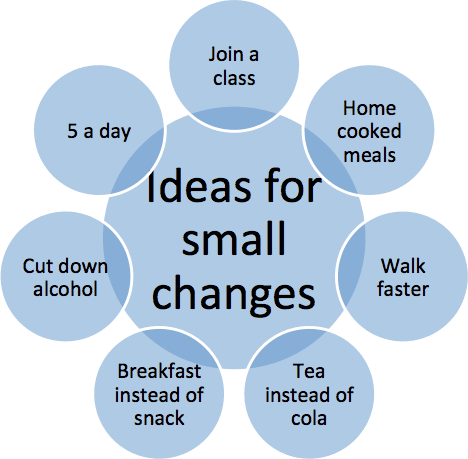
“I would echo what my practice nurse has said. For me the main issues were time, and being unsure of how to broach the topic. I have found it really effective to broach the issue and then to book them an appointment [addressing time pressures] either with me or our practice nurse who has also done this module. It has been really helpful for me to separate patients that require psychological support from those who need a hand with lifestyle changes [addressing role adequacy], and to concentrate on dietary change as patients always seem to have more barriers to exercise. I've now become more familiar with local resources and have found it really helpful to refer families with overweight children to our local specialist MEND service. I really now see that overweight and obesity are risk factors that need addressing or treating [role legitimacy], just as you would high blood pressure or smoking.”
The practise nurse
Jenny is an experienced practise nurse and already does a lot of counselling around dietary change as part of her diabetic clinic, but is less confident in extending this beyond that clinic. She explains:
“When I started raising the issue of obesity with my patients outside of my diabetes clinic, [addressing role adequacy] I thought it would be much more difficult than it actually was. If you ask in the right way, [addressing fear of offense] people are generally really grateful for the opportunity to talk about their issues. I have also found that the technical side of what advice we should be giving is actually very simple [addressing role adequacy]. The main thing is to really listen to your patient, and a goal will normally naturally arise from that conversation. The skill is turning that goal into a really achievable action plan and following it up. This has also improved my dietary counselling in diabetes – I still give information, but spend more time working through their problems.”