
John Barker
56, Male
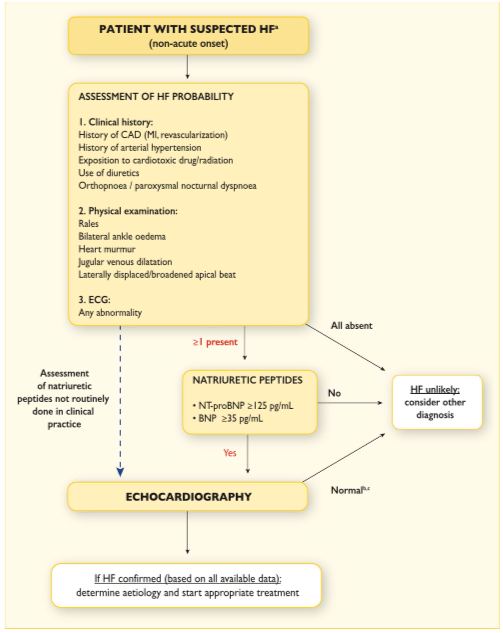
The most important initial investigations here are plasma BNP or NT-pro-BNP, ECG and echocardiogram.[1]
Click on the tabs below (and click headings to open and close the subpanels) to view the results and interpretation of the investigations.
B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-pro-BNP)
Explanation:
BNP is released by the myocardium in response to increased ventricular filling pressure. It has diuretic, natriuretic and antihypertensive effects through inhibition of the renin-angiotensin-aldosterone system. It also has systemic and renal sympathetic activity and may provide a protective effect against fibrosis and ‘adverse remodelling’ which occurs in progressive heart failure. Inactive proBNP is cleaved into biologically inert NT-pro-BNP and biologically active BNP, both of which can be measured. Patients with normal plasma BNP and/or NT-pro-BNP levels are unlikely to have heart failure. The test has a high negative predictive value and therefore a normal BNP represents a good screening investigation since it rules out heart failure (high sensitivity).
*Note there are other causes of elevated BNP such as renal failure, atrial fibrillation and high output states such as thyrotoxicosis which may give false positive results. So it is less good at ruling in heart failure (low specificity).
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| BNP | 300 | < 35 | pg/mL |
| NT pro-BNP | 1000 | < 125 | pg/mL |
12 lead ECG
Explanation:
An abnormal ECG increases the likliehood of the diagnosis of heart failure but has low specificity. Some ECG abnormalities provide information on aetiology (for example myocardial infarction) and some ECG findings direct therapy (for example anticoagulation in atrial fibrillation, cardiac resynchronisation therapy pacing if broad QRS complex). Patients with a completely normal ECG are unlikely to have heart failure. Therefore a normal ECG represents a screening investigation to rule out heart failure.
Results
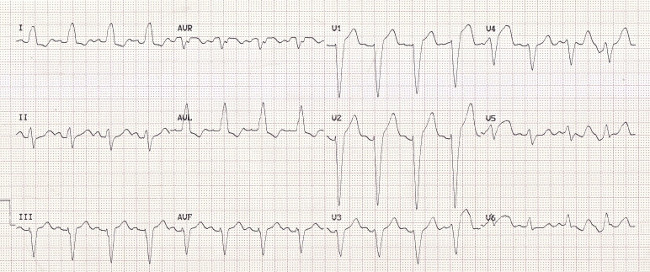
The ECG demonstrates sinus rhythm with broad left bundle branch block (QRS duration >120ms). This is potentially important for treatment. If he has severely impaired left ventricular function (LVEF ≤35%) and remains symptomatic once on optimal medical therapy, then he may be considered for cardiac resynchronisation therapy.
Echocardiogram
Explanation:
This measures the anatomical structures of the heart and how they move in the cardiac cycle. Echocardiography is the most useful widely available test in patients with suspected heart failure to establish the diagnosis. It provides immediate information on ventricular and atrial sizes, ventricular wall thickness, ventricular systolic and diastolic function, valve function, and pulmonary hypertension. The fraction of blood ejected during systole is known as left ventricular ejection fraction (LVEF) and this differentiates between the different types of heart failure (HFrEF LVEF <40%; HFmrEF LVEF 40-49%; HFpEF LVEF ≥50%). The echocardiogram can also be used to assess for left ventricular hypertrophy and/or atrial enlargement which are important features in HFmrEF and HFpEF. Assessment of diastolic function is possible. The presence of a wall motion abnormality may reflect prior myocardial infarction
Results
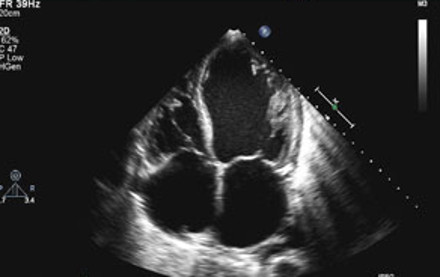
The echo demonstrates left ventricular dilatation with biatrial enlargement. Left ventricular systolic function is severely impaired (LVEF 32%). This is consistent with heart failure with reduced ejection fraction (HFrEF).
There is also a moderate central jet of mitral regurgitation (functional mitral regurgitation secondary to failure of mital valve leaflet coaptation due to ventricular dilatation which has stretched the mitral annulus).
Full blood count and iron studies
Explanation:
Iron deficiency is common in heart failure (as with other chronic illnesses). It may lead to anaemia and/or skeletal muscle dysfunction. Anaemia is more common in patients with renal impairment and advanced disease. This is associated with worse symptoms, functional status and prognosis as well as increased heart failure hospitalisations. Looking for an underlying cause for anaemia is important as this may allow treatment (for example intravenous iron treatment for iron deficiency anaemia).
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Haemoglobin | 110 | 115-165 | g/L |
| White cell count | 10.1 | 4-11 | x109/L |
| Neutrophils | 6.8 | 1.5-7.0 | x109/L |
| Platelets | 350 | 150-400 | x109/L |
| Serum ferritin | 82 | 30-300 * | µg/L |
| Transferrin saturation | 10% | 15-50 * | % |
Low haemoglobin with low serum ferritin and low transferrin saturation are consistent with anaemia and iron deficiency.
Renal function
Explanation:
Heart failure and chronic kidney disease (CKD) frequently coexist, share many risk factors (for example diabetes and hypertension) and interact to worsen prognosis. CKD is defined as eGFR <60 mL/min/1.73m2 and/or presence of albuminuria. Worsening renal function and large increases in serum creatinine (acute kidney injury) may occur with diuretic therapy and other nephrotoxic drugs.
Hypokalaemia and hyperkalaemia are associated with heart failure and the drugs used for heart failure treatment:
- Diuretics reduce serum potassium.
- Angiotensin-converting-enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB) and mineralocorticoid receptor antagonists (MRA) may increase serum potassium.
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Sodium | 141 | 137 - 145 | mmol/L |
| Potassium | 4.2 | 3.5 - 4.9 | mmol/L |
| Urea | 4.5 | 2.5 - 7.5 | mmol/L |
| Creatinine | 97 | 60 - 110 | µmol/L |
| Glomerular filtration rate (eGFR) | 45 | > 60 | mL/min/1.73m2 |
The eGFR is reduced consistent with underlying CKD.
Liver function tests
Explanation:
These may be disturbed in the presence of right sided heart failure.
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Protein | 75 | 61 - 76 | g/L |
| Albumin | 42 | 37 - 49 | g/L |
| Bilirubin | 20 | < 22 | µmol/L |
| Alaninine aminotransferase | 30 | 1 - 31 | U/L |
| Alkaline phosphatase | 65 | 45 - 105 | U/L |
| Gamma glutamyl transpeptidase | 34 | 4 - 35 | U/L |
The liver function tests are within normal limits.
C reactive protein
Explanation:
This is an acute phase of protein produced predominantly by the liver in response to inflammatory cytokines. Elevation is unlikely in heart failure and may therefore point towards an alternative diagnosis (such as pneumonia).
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| CRP | 4 | < 10 | mg/L |
This CRP level is normal.
Blood glucose
Explanation:
Diabetes is common in heart failure. Elevated plasma glucose and glycosylated-haemoglobin (reflecting glucose levels over the last two months) indicate diabetes.
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Glucose | 14 | Random < 11 | mmol/L |
| Glycosylated Haemoglobin | 7.2 | < 6 | % |
The glucose concentration and HbA1c are elevated consistent with underlying diabetes.
Cholesterol
Explanation:
The fasting lipid profile includes total cholesterol, low density lipoprotein (LDL) and high density lipoprotein (HDL).
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Total Cholesterol | 9.8 | < 5 | mmol/L |
This is elevated into the range typical of familial hypercholesterolaemia.
Thyroid function tests
Explanation:
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Thyroid stimulating hormone | 2.1 | 0.4 - 4.0 | mlU/L |
TFTs are within normal limits.
Chest X-ray
Explanation :
The chest x-ray is most useful for identifying an alternative cause of breathlessness (for example pneumonia or lung malignancy). However the chest X-ray may document the examination findings of pulmonary venous congestion and oedema. It may also demonstrate cardiomegaly but note that significant left ventricular dysfunction may be present without cardiomegaly.
Results
The ground glass appearance in the lower zones, with prominent upper lobe blood vessels, is typical of pulmonary oedema. Cardiomegaly is also noted.
Cardiac Magnetic Resonance Imaging (Cardiac MRI)
Explanation:
Cardiac magnetic resonance imaging is the gold standard for measurement of cardiac chamber volumes, ventricular function and ventricular mass. It is particularly useful in patients with poor echocardiographic windows. Late enhancement imaging of myocardial fibrosis allows differentiation between ischaemic and non-ischaemic causes of heart failure and permits assessment of myocardial viability in patients with coronary artery disease being considered for revascularisation. Stress perfusion imaging can also be used to look for significant underlying coronary atery disease.
Results
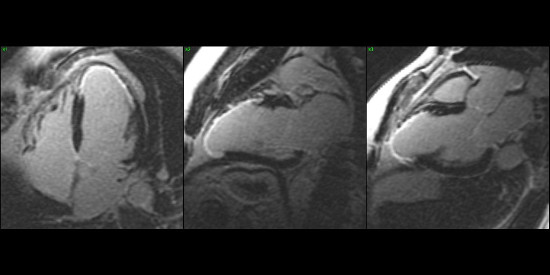
The cardiac MRI confirms the echocardiographic findings of left ventricular dilatation and severe systolic impairment (LVEF 32%). Late enhancement imaging demonstrates an ischaemic pattern of fibrosis anteroapically consistent with prior anterior myocardial infarction.
[1] Ponikowski P et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. The task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). European Heart Journal 2016;37:2129-2200.