Some of the relevant findings on examination and their physiological explanation are as follows:

John Barker
49, Male
Questions: Explain the following examination findings
Click on each title below to see the model answer...
Heart rate > 120bpm
Model answer:
The tachycardia is almost certainly the result of activation of the sympathetic nervous system. This has also caused peripheral vasoconstriction and sweating, giving rise to the cold and clammy hands. It is likely that the sympathetic nervous system has been activated by a reduction in cardiac output and the consequent relatively low blood pressure of 102/68. The fact that the blood pressure remains low despite the tachycardia and peripheral vasoconstriction suggests that despite compensatory mechanisms, organ perfusion may be compromised.
Crackles at the lung bases and possible third heart sound
Model answer:
The signs of activation of the sympathetic nervous system (see answer above under "Heart rate > 120bpm" ) are relatively non-specific. However, bilateral inspiratory basal crackles together with a third heart sound suggest a cardiac problem. Following coronary artery occlusion, the myocardium distal to the occlusion loses its blood supply and almost immediately stops contracting. If the volume of myocardium is large, the cessation of contraction can be sufficient to seriously compromise the performance of the whole heart. This results in a reduction in stroke volume that may be so marked that cardiac output cannot be restored by an increase in heart rate. Under this circumstance left atrial pressure increases and the Frank-Starling mechanism is brought into play to further increase stroke volume. However, with a large portion of the heart muscle not contracting, the left atrial pressure may increase substantially and this results in the transudation of fluid from the alveolar capillaries, resulting in pulmonary oedema and inspiratory crackles. The high left atrial filling pressure causes a sudden filling of the left ventricle when the mitral valve opens at the beginning of diastole, giving rise to the third heart sound.
Evidence of sympathetic activation, a third heart sound and pulmonary oedema all suggest a cardiac cause for the symptoms. Moreover, they indicate that a substantial portion of the myocardium has become ischaemic and is threatening to infarct.
Raised jugular venous pressure
Model answer:
The internal jugular vein is observed to assess central venous pressure. The most common cause of raised JVP is congestive cardiac failure, in which the raised venous pressure reflects right ventricular failure (see also longer explanation on the following page).
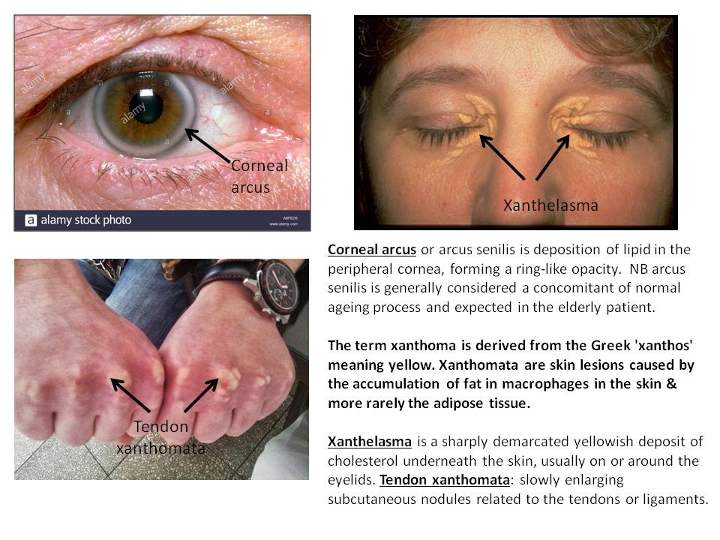
The presence of corneal arcus, xanthelasma and tendon xanthoma
Model answer:
The presence of a corneal arcus, xanthelasma and tendon xanthoma suggest hypercholesterolaemia. The strong positive family history of MI suggests that this is familial and tendon xanthoma (typically affecting the extensor tendons on the hands and the Achilles tendons) are virtually pathognomonic of familial hypercholesterolaemia (FH).