
John Barker
49, Male
Click on the tabs below to view the results and interpretation of these investigations.
Consider the questions for each section, asking you to interpret these investigations; click on the question panels to reveal model answers.
12 lead ECG
Explanation:
The presence of ST elevation indicates that an epicardial coronary artery has occluded and urgently needs to be opened. If the ECG is normal it should be repeated after 10 minutes. If changes are present on the ECG other than the ST elevation, a patient may still be having an MI but the advantages of immediate reperfusion are less well proven. The ECG is the first and most important investigation.
In practice, a patient admitted with a possible MI would have continuous ECG monitoring; this will indicate any disturbances of rhythm but a full 12 lead ECG is required for diagnosis.
Results
Questions: Click on each question panel below to see the model answer...
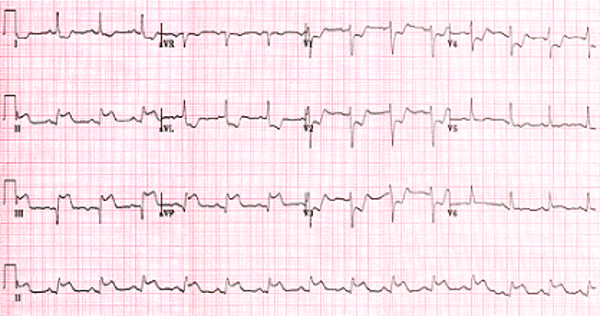
Question 1: Interpret the ECG
Model answer:
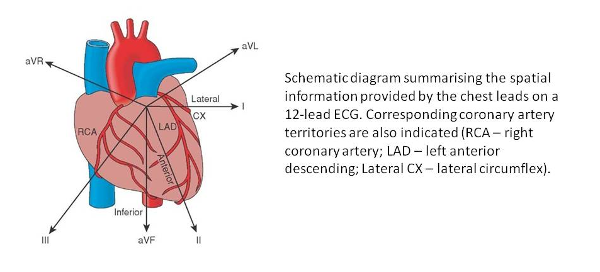
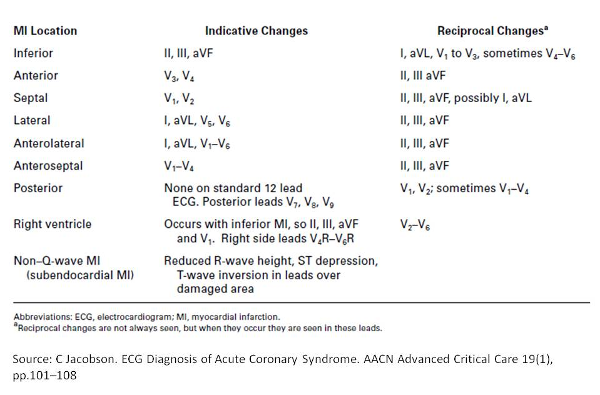
There is ST elevation in II, III and aVF. These changes are diagnostic of acute myocardial infarction (MI) on the inferior aspect of the heart i.e. this is an acute inferior myocardial infarction (refer to the figure & table of corresponding ECG changes below). Reciprocal ST depression (i.e. changes on the opposite side of the myocardium that is infarcting) in lead aVL & V1 is often seen in a large inferior MI.
Question 2: Which artery has become occluded?
Model answer:
Right coronary artery.
Inferior STEMI can result from occlusion of all three coronary arteries:
- The vast majority (~80%) of inferior STEMIs are due to occlusion of the dominant right coronary artery (RCA).
- Less commonly (around 18% of the time), the culprit vessel is a dominant left circumflex artery (LCx).
- Occasionally, inferior STEMI may result from occlusion of a “type III” or “wraparound” left anterior descending artery (LAD). This produces the unusual pattern of concomitant inferior and anterior ST elevation.
While both RCA and circumflex occlusion may cause infarction of the inferior wall, the precise area of infarction in each case is slightly different:
- The RCA territory covers the medial part of the inferior wall, including the inferior septum.
- The LCx territory covers the lateral part of the inferior wall and the left posterobasal area.
This produces subtly different patterns on the ECG:
- The injury current in RCA occlusion is directed inferiorly and rightward, producing ST elevation in lead III > lead II (as lead III is more rightward facing).
- The injury current in LCx occlusion is directed inferiorly and leftward, producing ST elevation in the lateral leads I and V5-6.
Serum Troponin levels (Blood test)
Explanation:
Troponins I and T are specific to cardiac muscle and are the favoured biomarkers to diagnose myocardial inforaction and also other forms of myocardial injury.
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| Troponin T | 28 | < 14 | ng/L |
Questions: Click on the question panel below to see the model answer...
Question: Interpret the Troponin T result:
Model answer:
Troponin T is elevated. An elevated Troponin T of this level, in combination with cardiac chest pain and changes compatible with acute myocardial ischaemia on ECG is diagnostic of acute myocardial infarction.
Creatine kinase, cardiac troponin I and cardiac troponin T are intracellular proteins released from dead heart muscle cells. Creatine kinase exists in a variety of cells particularly skeletal muscle and so is now rarely used to diagnose myocardial infarction.
Cardiac troponin I and cardiac troponin T are biological markers of cardiac muscle death (cardiomyocyte necrosis). They are released into the circulation when damage to cardiac muscle has occurred. Troponins C, I and T form the troponin‑tropomyosin complex which is responsible for regulating cardiac muscle contraction. Troponins I and T are the recommended biomarkers for diagnosing myocardial infarction (MI) in “Chest pain of recent onset” (NICE clinical guideline 95), when a rise and fall in troponin levels can signify that myocardial damage has occurred. The optimum sensitivity of non‑high‑sensitivity troponin assays for acute MI occurs 10–12 hours after the onset of symptoms. For many people, this results in the need for hospital admission and observation while serial troponin testing is carried out. To overcome this, high‑sensitivity troponin assays have been developed. These are able to detect lower levels of troponin in the blood earlier than older standard assays, leading to improved early detection of acute MI.
Using these high-sensitivity assays enables earlier detection of changes in troponin levels. Locally at Guy’s & St Thomas’s Hospital, an interval high sensitivity cardiac troponin test is usually performed at +3hours. This allows non-ST-segment elevation myocardial infarction (NSTEMI) to be ruled out within 4 hours. The increased sensitivity of these assays could mean a shorter inpatient hospital stay for people without raised levels of troponin and earlier intervention for those with a confirmed NSTEMI. As with older standard troponin assays, the high-sensitivity assays are intended to be used with clinical history taking and the electrocardiogram to diagnose NSTEMI because, despite being highly specific for cardiomyocyte necrosis, troponin may also be raised in people who do not have underlying evidence of ischaemic heart disease. Conditions other than acute MI that may cause troponin levels to be raised include myocarditis, congestive heart failure, severe infections, musculoskeletal conditions and renal disease.
[Source: https://www.nice.org.uk/guidance/dg15/chapter/3-clinical-need-and-practice]
Chest X-ray
Explanation:
The chest X-ray is useful to document the examination findings of pulmonary oedema. In addition, there may be evidence of another cause of chest pain such as air in the mediastinum (oesophageal rupture) or aortic dissection (widened mediastinum, pleural effusions).
Results
Questions: Click on the question panel below to see the model answer...
Question: What does the chest x-ray show?
Model answer:
A ground glass appearance in the lower zones, with prominent upper lobe blood vessels, is typical of cardiogenic pulmonary oedema.