James
69, Male
Approach to motor disorders: basic concepts
The neurologist looks for patterns of functional abnormality. These represent features consistent either with lesions in neuronal systems, including nuclei and their interconnecting pathways (e.g. a median nerve palsy), or with disease syndromes. With respect to the latter, clinicians often differentiate between “lower motor neurone syndromes” and “upper motor neurone syndromes”, and between “pyramidal” and “extra-pyramidal” disorders.
A Note on “Lower” and “Upper” Motor Neurone Syndromes
Lower and upper motor neurone syndromes are clinical rather than anatomical entities. These terms are used to describe patterns of functional abnormality that help to localise a neurological lesion at or below the anterior horn cell (“lower motor neurone lesion”), or above the anterior horn cell (“upper motor neurone lesion”).
Remember that a motor neurone is the efferent nerve that directly innervates skeletal muscle. These correspond to the “lower” motor neurones in the functional description. (So “lower” is actually a redundant term here).
The term “upper motor neurones” is used by clinicians to describe cortico-spinal interneurons that arise from the motor cortex and descend to the spinal cord, where they activate the lower motor neurons through synapses. So these neurones synapse with other neurones - they do not directly innervate skeletal muscle. They are not motor neurones by definition. Hence, in strict anatomical/physiological terms, there is no such thing as an “upper motor neurone”!
However, the clinical patterns of “lower” and “upper” motor neurone weakness are useful when localising the lesion to at/below (lower), or above (upper) the anterior horn cell through the pattern of neurological signs that result, and so the terms still persist in clinical practice.
Lower Motor Neurone (LMN) Signs
Indicate that the lesion is either in the anterior horn cell or distal to the anterior horn cell (i.e. anterior horn cell, root, plexus, peripheral nerve).
Characterised by decreased muscle tone, weakness and wasting (atrophy) in the muscle(s) supplied by that motor nerve, arreflexia (absence of the relevant reflex - the motor nerve is the efferent arm of the reflex arc), muscle fasciculations.
Again the level of the problem can generally be inferred from accompanying symptoms and signs, for example:
- Back pain and sciatica suggests a root problem
- Weakness of the biceps with absence of the biceps reflex, with upper motor neurone signs in the legs suggests cord disease (eg a disc) at C5/6 (LMN at that level, UMN below).
- Weakness of thumb abduction, wasting of the thenar eminence and numbness in the thumb and lateral 21/2 fingers suggests median nerve pathology.
Upper Motor Neurone (UMN) Signs
Indicate that the lesion is above the anterior horn cell (i.e. spinal cord, brain stem, motor cortex).
Are characterised by increased muscle tone (spasticity), weakness (generally flexors weaker than extensors in the legs and the reverse in the arms - pyramidal pattern of weakness), increased reflexes, an up-going plantar response and sustained clonus (a few beats is normal).
Can be further localised by the other symptoms that go along with the weakness. For example:
- A cord lesion may also cause sphincter symptoms, a sensory level, bilateral motor signs.
- A brain stem lesion may also cause dysarthria, dysphagia, Horner's syndrome, cerebellar signs, spinothalamic sensory loss.
- A lesion of the motor cortex may be associated with frontal signs, dysphasia, hemianopia, disturbance of higher sensory function eg agnosias.
Extrapyranidal Disorders
The extrapyramidal system consists of those parts of the nervous system, excluding the motor cortex and corticospinal pathways, which are concerned with movement and posture.
Includes the basal ganglia, the subthalamic nuclei, the substantia nigra and other structures in the brainstem.
The accompanying symptoms and signs may provide clues as to the site of the lesion, for example:
- Intention tremor, dysmetria (past-pointing), dysdiadochokinesia and nystagmus suggest a cerebellar problem
- Resting pill-rolling tremor, cogwheel ragidity and bradykinesia suggest a lesion of the substantial nigra (Parkinsonism).
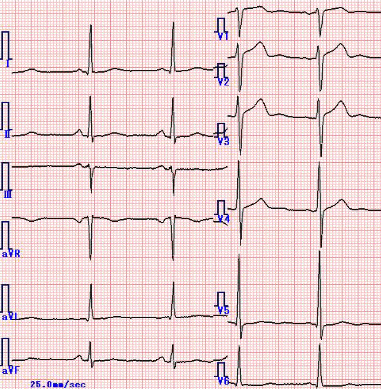
Cardiological Investigations
| Investigation Name | Investigation Result |
|---|---|
| ECG | The ECG showed sinus rhythm with no evidence of myocardial infarction but evidence of LVH.
|
| ECHO | The ECHO showed LVH but no valvular abnormality . |