
Bashir Agim
75, Male
The working diagnosis of leaking AAA is confirmed by the FAST scan and the CTA. The initial management is the same as any acutely unwell patient:
- Airway patent and administer oxygen
- Breathing spontaneously
- x2 large bore IV cannulae, crossmatch 10 units of blood and urgently contact blood bank.
Do not give IV fluids whilst the patient is alert and talking to you regardless of the blood pressure. If the patient becomes drowsy and the blood pressure is low then hypotensive resuscitation can commence whereby fluids are administered to support the blood pressure but not pushed aggressively, to avoid disturbing the haematoma at the site of the rupture.
The vascular surgical on call team should be contacted immediately as well as the anaesthetic on-call team and the emergency theatre co-ordinator. The patient will need immediate surgery and the vascular surgeon will review the patient and the images and decide on an endovascular, or open, approach to repair the leaking AAA.
-
Abdominal aortic aneurysm
An abdominal aortic aneurysm is where the abdominal aorta has enlarged to over 1.5 times the normal size of the aorta. Aortic aneurysms can develop anywhere in the aorta but the most common site is infrarenal and can extend to involve the iliac arteries.
The most common cause of AAA is atherosclerosis secondary to smoking. This causes weakening of the aortic wall and the media layer breaks down leading to aortic dilatation. AAA are fusiform or spindle shaped but they can also be saccular shaped (which is an outpouching of the aortic wall).
The natural progression of an AAA is to continue to enlarge and it becomes life-threatening if it ruptures. In the UK, repair is recommended when the maximum diameter of the abdominal aorta reaches 5.5cm. Most AAA are asymptomatic until they rupture, typical symptoms of which are outlined below.
-
Symptoms of a rupture AAA
- Sudden onset back pain/loin pain with collapse/fainting
- Pulsating sensation in the abdomen
- Central abdominal pain
-
Risk factors and causes
- Smoking
- Men age 65 or over – AAA are six times more common in men than women. There is a national screening programme where men over age of 65 are invited for an ultrasound scan to assess for an AAA
- Family History – you are four times more likely to have an AAA if a first degree relative has an AAA
- Collagen deficiency – Marfans/Ehlers-Danlos
- Hypertension – this can double your risk of a AAA
- Post-trauma
- Arteritis
- Mycotic infection
-
Management
AAA smaller than 5.5cm are under a surveillance programme and are monitored with regular ultrasound scans until they reach threshold size. In the interim, risk factors should be reduced such as stop smoking, good blood pressure control, cholesterol reduction, good diabetes control, regular exercise, weight loss and a healthy diet.
Surgery can be an open or endovascular approach depending on the patient’s fitness for surgery, anatomy of the aneurysm and patient’s choice. The open approach involves a midline incision in the abdomen, the aorta is clamped ideally infrarenal to limit renal ischaemia. The AAA is incised and old clot removed and the aorta is replaced with a synthetic graft which is sutured in place.
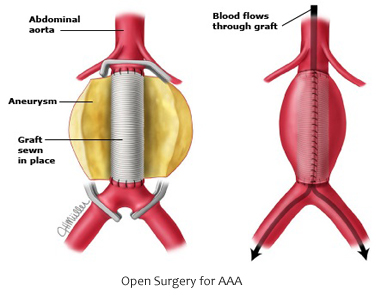
Figure 8. Open surgery for AAA
[SOURCE: from http://www.uptodate.com/contents/open-surgical-repair-of-abdominal-aortic-aneurysm ]The endovascular aneurysm repair (EVAR) can be performed under local anaesthetic/spinal anaesthetic or general anaesthetic. It is a good approach for frail and elderly patients. It also requires a few criteria to be met namely that there is an infrarenal neck of at least 15mm from the lowest renal artery to allow the stent graft to be placed in healthy aorta and a diameter of no more than 30mm. In the endovascular approach the stent is passed through the femoral artery over a wire to the infrarenal aorta where it is placed in position under X-ray guidance. Most patients stay in hospital for 1-3 days after EVAR and recovery is shorter than with open repair.
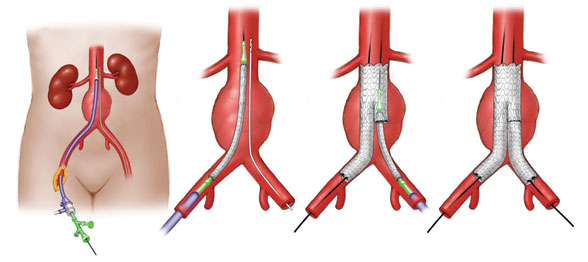
Figure 9. AAA treatment 
Figure 10. EVAR before and after
(A) Invasive angiography prior to endovascular repair (EVAR): rupture of an infrarenal AAA.
(B) Final angiography after EVAR: successful exclusion of the ruptured AAA by a bifurcated stent graft; no endoleak visible
[SOURCE: from https://www.researchgate.net/publication/277262501_The_Abdominal_Aortic_Aneurysm_and_Intraluminal_Thrombus_Current_Concepts_of_Development_and_Treatment ]