3] Assessment of the Film
3.4] Pleura
The pleura is normally invisible. It can be seen however if the pleural space becomes filled with air, fluid including blood or fluid or solid material.
Air in the pleural space (Pneumothorax)
- Look for lack of pleural markings up to the chest wall
- Look for a pleural edge
- Look for one lung to appear blacker than the other
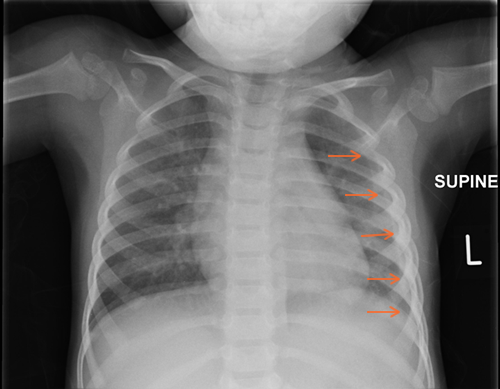
If air gets into the pleural space, the underlying lung collapses. Signs to look for include lack of pleural markings to the chest wall, a pleural line demarking the edge of the lung and one lung may look blacker than the other side.
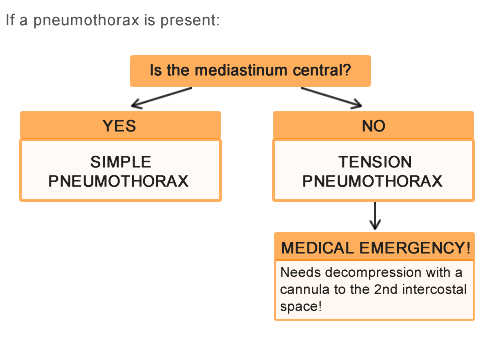
If a pneumothorax is present
If a pneumothorax is present, the nature of it has to be decided. The mediastinum needs to be assessed and if it remains central it is likely to be a simple pneumothorax. If the mediastinum is shifted over to the other side from the pneumothorax, a tension pneumothorax is present. This is a Medical emergency as it can compromise venous return to the heart. It needs immediate decompression with a cannula placed in the second intercostal space on the side of the pneumothorax. This releases the air under tension and may be accompanied by a ‘hiss’ noise.
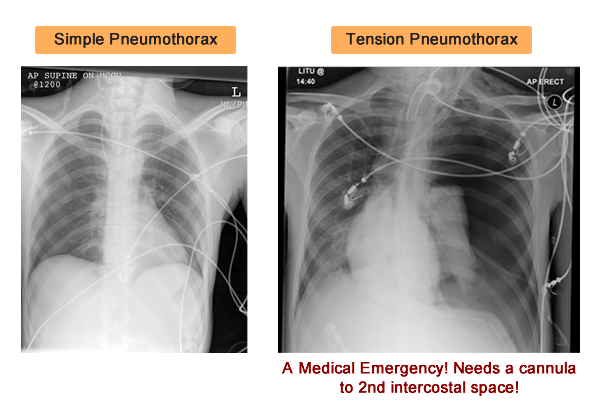
Examples
Here are examples of CXR’s of a simple and tension pneumothorax.
Fluid in the pleural space (Pleural Effusion)
To assess the film for a pleural effusion, i.e. fluid in the pleural space look for these signs.
- Look for increased density peripherally
- Look for mediastinal shift (to contralateral side)
- Look for a meniscus
- Look for blunting of the costophrenic angle
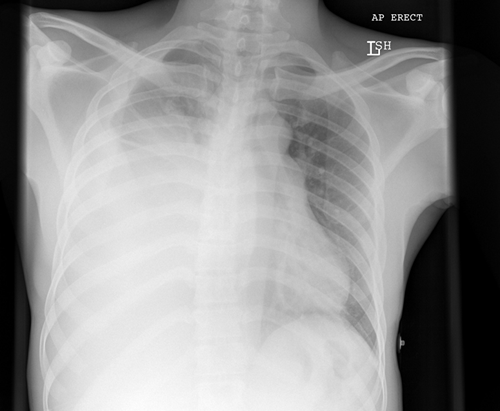
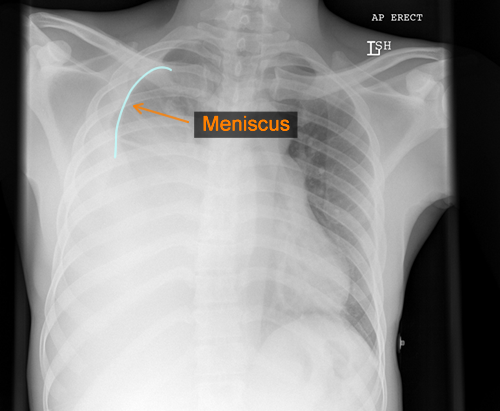
Here is an example on a CXR of a right sided pleural effusion. You can see the meniscus of the effusion tracking up the right chest wall.
Solid (Pleural thickening)
Pleural thickening can be seen on a CXR as similar increased density peripherally but has no associated meniscus or mediastinal shift. It can be difficult to differentiate from an effusion and often persists for weeks after an effusion.
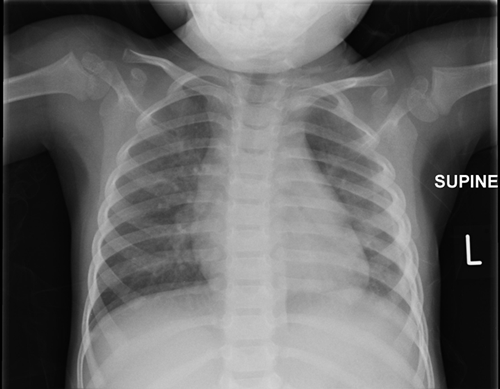
Here is an example of pleural thickening seen on a CXR which is seen as residual change after the child has been treated for a chest effusion (known as an empyema when infected and filled with pus).
A diagram to show both hila. The left hilum can be up to 1.5cm higher than the right hilum.