James Bailey
21, Male
Immediate investigations to confirm the diagosis and assess severity
Click on the tabs below to view the results and interpretation of these investigations.
Consider the questions for each section, asking you to interpret these investigations; click on the question panels to reveal model answers.
Chest X-ray
Results

Questions: Click on the question panel below to see the model answer...
Question: What does James' chest x-ray show?
Model answer:
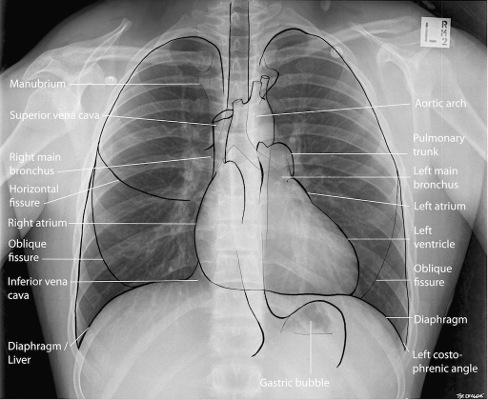
James’s chest x-ray: hyperinflated lung fields (> 6 ribs visible anteriorly, flattened hemidiaphragms). Lung fields clear. No pneumothorax. (The two white circles bilaterally in the upper lung fields are ECG skin electrodes).
Chest X-ray is not routinely recommended in patients in the
absence of:
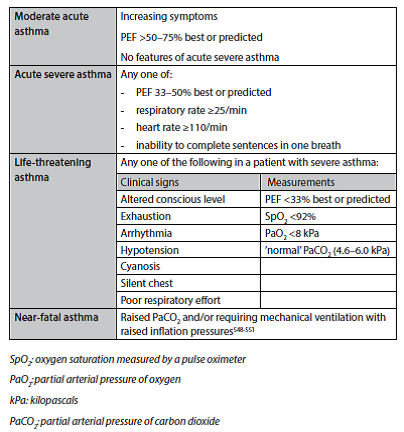
James has features of life-threatening asthma (see Table 1: “Clinical features used to grade the severity of an acute asthma attack”)
In acute asthma, the chest x-ray may be normal but may show hyperinflation in severe cases. This may be evidenced by:
- a. Flattened hemidiphragms.
- b. Hyperlucent lungs ( less bronchovascular markings per cm 2)
- c. More than 6 anterior or 10 posterior ribs in the mid-clavicular line.
The chest x-ray will investigate for complications of asthma (pneumothorax, pneumomediastinum, subcutaneous emphysema).
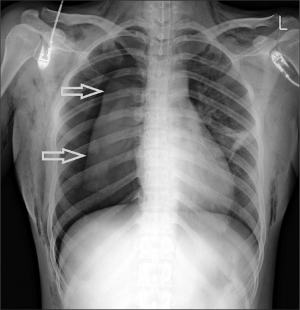
By means of example, the chest x-ray below illustrates two of the potential complications of acute severe asthma: Pneumothorax + subcutaneous emphysema.
Peak expiratory flow rate (PEFR)
Results
PEFR = 170 L/min
(James’ predicted PEFR = 595 L/min)
Questions: Click on each question panel below to see the model answer...
Question 1: Interpret the PEFR result
Model answer:
PEFR = 170 L/min, compared to a predicted PEFR = 595 L/min, means that James’ PEFR is 28.6% of the predicted PEFR value.
This is cause for concern because PEFR<33% predicted is an indicator of life-threatening asthma.
Question 2: Why is the PEFR low in an acute asthma attack?
Model answer:
Peak Expiratory Flow Rate:
In an acute asthma attack, acute bronchoconstriction will increase airway resistance and result in a reduction in the peak expiratory flow rate.
The magnitude of the reduction in PEFR is a useful objective indicator of the severity of the asthma attack, in combination with other clinical features. See Table 1: Asthma Severity Grading
Arterial blood gases (ABG)
Results
| Investigation Name | Investigation Result | Normal Range | Units |
|---|---|---|---|
| PaO2 | 7.2 | 11 - 13.5 | kPa |
| PaCO2 | 3.8 | 4.6 - 6 | kPa |
| pH | 7.47 | 7.35 - 7.45 | |
| [H+] | 34 | 35 - 45 | nmol/L |
Questions: Click on the question panel below to see the model answer...
Question: Interpret the arterial blood gas result:
Model answer:
There is significant hypoxaemia and a respiratory alkalosis (pH is high, PaCO2 is low indicating that the alkalosis us of respiratory origin).
The low PaCO2 is helpful in confirming that James is maintaining alveolar ventilation and a high level of neural respiratory drive – he is not yet exhausted. Beware of a normal, and especially a raised, PaCO2 in a patient with acute asthma!
PaO2 < 8kPa without CO2 retention: “Type 1 respiratory failure” (Type 2 respiratory failure is when hypoxaemia is accompanied by hypercapnia i.e. alveolar hypoventilation)
Patients with SpO2 <92% (irrespective of whether the patient is on air or oxygen) or other features of life-threatening asthma require ABG measurement. SpO2 <92% is associated with a risk of hypercapnia. Hypercapnia is not detected by pulse oximetry. In contrast, the risk of hypercapnia with SpO2 >92% is much less.