
James Bailey
21, Male
View Table 2 and then consider the questions beneath it as to intial drug treatment and the effects of salbutamol
Table 2: Management of acute asthma in adults in hospital
You may also access this table as a PDF version here.
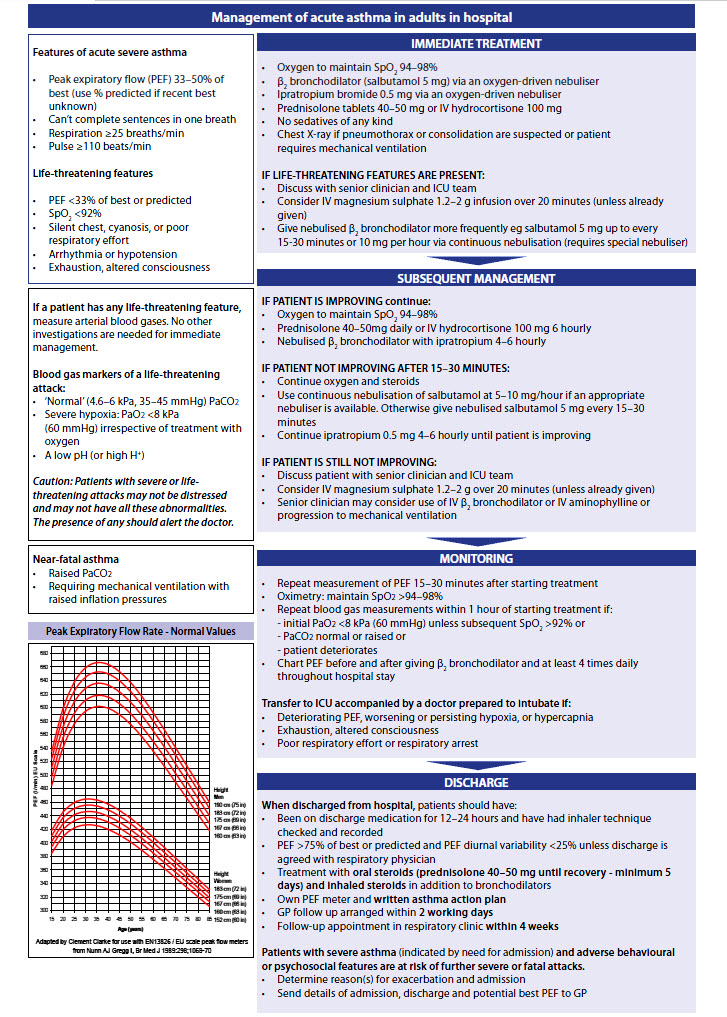
[Source: SIGN 158: British guideline on the management of asthma (2019)]
Consider these Questions as to intial drug treatment and the effects of salbutamol
Click on each title below to see the model answer...
Q1. What initial drug treatment would you recommend for James?
Drug treatment of acute asthma:
Oxygen
Give controlled supplementary oxygen to all hypoxaemic patients with acute severe asthma titrated to maintain an SpO2 level of 94–98%. Give high concentrations, up to FiO2 100%. Do not delay oxygen administration in the absence of pulse oximetry but commence monitoring of SpO2 as soon as it becomes available.
High-dose inhaled short-acting β2 adrenoreceptor agonist bronchodilators
e.g. nebulised salbutamol 5mg or terbutaline 10mg via oxygen-driven nebuliser. Repeat doses of β2 agonists at 15–30 minute intervals or give continuous nebulisation of salbutamol at 5–10 mg/hour (requires the appropriate nebuliser) if there is an inadequate response to initial treatment.
Use high-dose inhaled β2 agonists as first-line agents in patients with acute asthma and administer as early as possible. Reserve intravenous β2 agonists for those patients in whom inhaled therapy cannot be used reliably.
Nebulised ipratropium bromide (nebulised anti-cholinergic)
Add nebulised ipratropium bromide (0.5 mg 4–6 hourly) to β2 agonist treatment for patients with acute severe or life-threatening asthma, or those with a poor initial response to β2 agonist therapy.
Combining nebulised ipratropium bromide with a nebulised β2 agonist produces significantly greater bronchodilation than β2 agonist alone, leading to faster recovery and shorter duration of admission. Anticholinergic treatment is not necessary and may not be beneficial in milder asthma attacks or after stabilisation.
Systemic glucocorticoids (corticosteroids)
Corticosteroids reduce mortality, relapses, subsequent hospital admission and requirement for β2 agonist therapy. The earlier they are given in the acute attack the better the outcome.
Prednisolone 40–50 mg daily or intravenous hydrocortisone 400 mg daily (100 mg six-hourly) are as effective as higher doses. Give orally unless patient is unable to swallow (no benefit of iv hydrocortisone over prednisolone otherwise).
Continue prednisolone (40–50 mg daily) for at least five days or until recovery.
Intravenous magnesium sulphate
Consider giving a single dose of IV magnesium sulphate to patients with acute severe asthma (PEF <50% best or predicted) who have not had a good initial response to inhaled bronchodilator therapy. Magnesium sulphate (1.2–2 g IV infusion over 20 minutes) should only be used following consultation with senior medical staff.
Q2a. What class of drug is salbutamol?
Model answer:
Salbutamol is a highly selective β2-adrenoreceptor agonist.
Q2b. What is the mechanism of action of salbutamol?
Model answer:
After inhalation, approximately 10 – 20% of the inhaled dose of salbutamol reaches the lung (majority, c80%, is deposited in oropharynx, will be swallowed into the gut), in lung onset of action is within 3 -5 minutes, peaking at 15 -20 minutes.
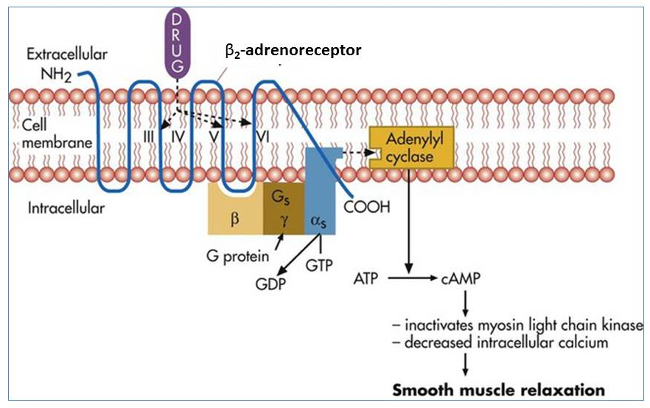
Salbutamol is a beta-2-adrenoreceptor agonist that bronchodilates by relaxing airway smooth muscle. Beta-2-adrenoreceptor agonist activation leads to activation of a stimulatory G protein bound to the intracellular side of the cell membrane. Adenyl cyclase is activated by the G protein, which increases the synthesis of 3’-5’-cyclic adenosine monophosphate (cAMP) from adenosine triphosphate (ATP). cAMP causes smooth-muscle relaxation by inactivating myosin light chain kinase, which is an enzyme that causes smooth-muscle contraction. Increased cAMP also inhibits intracellular calcium release, leading to relaxation of airway smooth muscle and decreasing the sensitivity of contractile proteins.
Q2c. What are the potential side-effects of salbutamol?
Model answer:
Up to approximately 10% of patients can be expected to experience adverse reactions. These depend upon the dose and the individual sensitivity. Most commonly reported are restlessness, fine tremor (usually of hands), dizziness, nausea, taste alteration. Tachycardia/cardiac arrhythmias, paradoxical bronchospasm and hypokalaemia are important in the acute setting.
The table below presents possible adverse drug reactions for salbutamol in system organ class order and sorted by frequency:
Organ System |
Frequency |
Adverse drug reaction |
Immune system disorders |
Very rare (including isolated cases) (<1/10,000) |
Hypersensitivity reaction |
Metabolism |
Rare ( >1/10,000, <1/1,000) |
Hypokalaemia, hyperglycaemia |
Psychiatric disorders |
Common (>1/100, <1/10) |
Restlessness |
Nervous system disorders |
Common (>1/100, <1/10) |
Fine tremor, dizziness |
Rare ( >1/10,000, <1/1,000) |
Hyperactive behaviour |
|
Very rare (including isolated cases) (<1/10,000) |
Hyperexcitability, sleeping disturbances, hallucinations |
|
Cardiac disorders |
Rare ( >1/10,000, <1/1,000) |
Tachycardia, cardiac arrhythmia (atrial fibrillation, supraventricular tachycardia, extrasystoles), palpitations, angina pectoris, blood pressure effects (lowering or increase) |
Unknown* |
Myocardial ischemia |
|
Vascular disorders |
Rare ( >1/10,000, <1/1,000) |
Peripheral vasodilation |
Very rare (including isolated cases) (<1/10,000) |
Collapse |
|
Respiratory, thoracic and mediastinal disorders |
Rare ( >1/10,000, <1/1,000) |
Paradoxical bronchospasm |
Gastrointestinal disorders |
Common (>1/100, <1/10) |
Nausea, taste alteration |
Skin and subcutaneous tissue disorders |
Common (>1/100, <1/10) |
Pruritus, rash, erythema, urticaria, angioedema |
Very rare (including isolated cases) (<1/10,000) |
||
Musculoskeletal disorders |
Rare ( >1/10,000, <1/1,000) |
Muscle cramps |
General disorders and administration site condition |
Common (>1/100, <1/10) |
Headache, application site reaction (mouth and throat irritation, burning sensation of the tongue) |