
Katie Tang
32, Female
The main findings on examination and their physiological explanation are as follows:
Explanation of physical findings:
- PE may be completely asymptomatic and be discovered incidentally during diagnostic work-up for another disease or at autopsy.
- Physical examination is often non-specific with respect to symptoms and signs, as shown in a multicentre, emergency medicine, pulmonary embolism registry. Despite this, when the clinical presentation is suspicious for PE, it should prompt further objective testing to confirm the diagnosis.
- In most patients, PE should be suspected based on the presence of dyspnoea, chest pain, presyncope or syncope, and/or haemoptysis.
- Chest pain is a frequent symptom and is usually caused by pleural irritation due to distal emboli causing pulmonary infarction.In central PE (in which the thrombus is in the main, left, or right pulmonary artery) angina-like chest pain may be present, possibly due to ischaemia of the right ventricle. This presentation requires differentiation from acute coronary syndrome or aortic dissection.
- Syncope is infrequent, but may occur regardless of the presence of haemodynamic instability.
- Other signs include fever, cough, or unilateral swelling/tenderness of a calf if a DVT is present. Shock (e.g., hypotension, tachycardia, tachypnoea) is a rare, but important, clinical presentation as it indicates central PE and/or a severely reduced haemodynamic reserve.
- If the PE has caused cor pulmonale, the patient may present with elevated jugular venous pressure, sternal heave, or accentuated pulmonary component of S2, although this is uncommon
Cor Pulmonale
- Shock
The patient can present with tachycardia and hypotension due to a reduced left ventricular cardiac output in the setting of right ventricular failure. - Sternal Heave
Physical findings may reflect the underlying lung disease or pulmonary hypertension, right ventricular hypertrophy (RVH), and RV failure. RVH is characterized by a left parasternal or subxiphoid heave. An increase in chest diameter, laboured respiratory efforts with retractions of the chest wall. - Elevated JVP
Distended neck veins with prominent a or v waves, may be seen. - Accentuation of P2
Splitting of the second heart sound with accentuation of the pulmonic component can be heard in the early stages. Other findings upon auscultation of the cardiovascular system may be RV third and fourth sounds or the systolic murmur of tricuspid regurgitation. - Abdominal findings
Hepatojugular reflux and pulsatile liver are signs of RV failure with systemic venous congestion. - Peripheral oedema
Examination of the lower extremities reveals evidence of pitting edema. Edema in cor pulmonale is strongly associated with hypercapnia.
Basic Science
Knowledge of bronchovascular anatomy (seen in the image below) is the key to the accurate interpretation of CT scans obtained for the evaluation of pulmonary embolism. A systematic approach in identifying all vessels is important. The bronchovascular anatomy has been described on the basis of the segmental anatomy of lungs. The segmental arteries are seen near the accompanying branches of the bronchial tree and are situated either medially (in the upper lobes) or laterally (in the lower lobes, lingula, and right middle lobe).
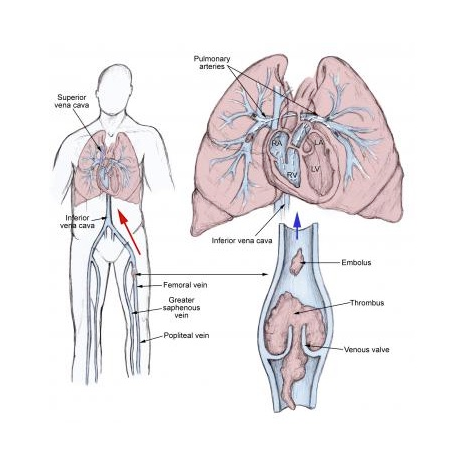
Pulmonary thromboembolism is not a disease in and of itself. Rather, it is a complication of underlying venous thrombosis. Under normal conditions, microthrombi (tiny aggregates of red cells, platelets, and fibrin) are formed and lysed continually within the venous circulatory system. This dynamic equilibrium ensures local hemostasis in response to injury without permitting uncontrolled propagation of clot.
Haemodynamic Compromise
Pulmonary embolism reduces the cross-sectional area of the pulmonary vascular bed, resulting in an increase in pulmonary vascular resistance, which, in turn, increases the right ventricular afterload. If the afterload is increased severely, right ventricular failure may ensue. In addition, the humoral and reflex mechanisms contribute to the pulmonary arterial constriction. Following the initiation of anticoagulant therapy, the resolution of emboli usually occurs rapidly during the first 2 weeks of therapy; however, it can persist on chest imaging studies for months to years. Chronic pulmonary hypertension may occur with failure of the initial embolus to undergo lysis or in the setting of recurrent thromboemboli.